What is antibiotic prophylaxis or “premedication” for a dental procedure? How do I know if it applies to me?
Antibiotic prophylaxis, or premedication, refers to giving a patient a loading dose of antibiotics in preparation for a dental surgical procedure, dental hygiene visit or other dental treatment dealing with the teeth or gums. During some dental treatments, bacteria your mouth can enter your bloodstream. In most people, the immune system kills these bacteria. But in some patients, bacteria from the mouth can travel through the bloodstream and cause an infection somewhere else in the body. Antibiotic prophylaxis, or dental premedication may offer these patients extra protection. Patients that normally require antibiotic prophylaxis have fallen under 2 categories: those with joint replacements or certain heart conditions. Some other health issues such as breast implants, brittle diabetics or organ transplant patients may require dental premedication, based on a physician’s recommendations.
Up until 2012, antibiotics were recommended for two years after joint replacement surgery or for a lifetime. Since that time, physicians and dentists have become more concerned about the potential harm of antibiotics including risk for anaphylaxis (allergic reaction), antibiotic resistance, and opportunistic infections such as Clostridium difficile (C-diff) were included in creating the new recommendation.
The 2015 American Dental Association stated that “In general, for patients with prosthetic joint implants, prophylactic antibiotics are NOT recommended prior to dental procedures to prevent prosthetic joint infection.” However, many orthopedic surgeons are still recommended premedication with antibiotics for their patients for 2 years or a lifetime. In patients with a history of complications associated with their joint replacement surgery, prophylactic antibiotics or premedication with antibiotics should be considered after consultation with the patient and orthopedic surgeon.
If you have a joint replacement and are unsure whether you should premedicate for your dental appointments or not, it is best to contact your orthopedic surgeon to determine what is best for you.
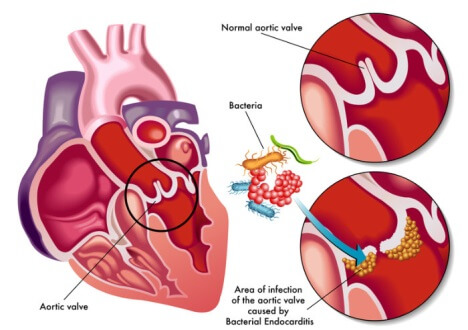
In patients with certain heart conditions, dental premedication is recommended to avoid infective endocarditis. Infective endocarditis (IE), also called bacterial endocarditis (BE), is defined as an inflammation of the endocardial surface of the heart. Endocarditis generally occurs when bacteria or other germs from another part of the body enter and spread through the bloodstream and attach to damaged areas in the heart. If left untreated, endocarditis can damage or destroy the heart valves and can lead to life-threatening complications.
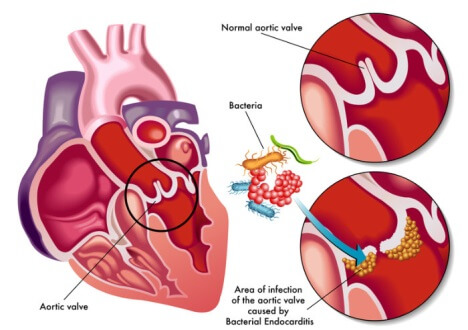
The American Heart Association says that premedication for dental procedures is required for the following conditions:
- “A prosthetic heart valve or who have had a heart valve repaired with prosthetic material.
- A history of endocarditis.
- A heart transplant with abnormal heart valve function.
- Certain congenital heart defects including:
- Cyanotic congenital heart disease (birth defects with oxygen levels lower than normal) that has not been fully repaired, including children who have had a surgical shunt and conduits.
- A congenital heart defect that’s been completely repaired with prosthetic material or a device for the first six months after the repair procedure.
- Repaired congenital heart disease with residual defects, such as persisting leaks or abnormal flow at or adjacent to a prosthetic patch or prosthetic device.”
Patients that have had stents placed in their hearts or a history of coronary artery bypass surgery no longer require to premedicate with antibiotics prior to dental procedures under the American Heart Association’s guidelines. Numerous scientific evidence concluded that the risk of adverse reactions to antibiotics generally outweighs the benefits of prophylaxis for many patients who would have been considered eligible for prophylaxis in previous guidelines. Concern about the development of drug-resistant bacteria also was a factor for the simplified guidelines.
The 2014 American Dental Association & American College of Cardiology guidelines add that optimal oral health is maintained through regular professional dental care and the use of appropriate dental products, such as manual, powered, and ultrasonic toothbrushes; dental floss; and other plaque-removal devices.
Antibiotic dosage and schedule
- 1 hour before the procedure to allows the antibiotic to reach adequate blood levels. However, if the dosage of antibiotic is inadvertently not administered before the procedure, the dosage may be administered up to 2 hours after the procedure.
- Patients not allergic to penicillin: oral amoxicillin 2g (50 mg/kg for children)
- Patients allergic to penicillin or ampicillin: oral cephalexin 2g (50 mg/kg for children) or clindamycin 600 mg (20 mg/kg for children)
If you have questions about whether you need to premedicate for your dental procedures, we will be happy to answer any questions you may have. It is best to carefully consider this matter with both you and your physician or surgeon and we are always happy to communicate with both. Contact us today 727-586-2681 with any questions.