Fixed Bridge
A bridge is an option when there are teeth on either side of the missing tooth.
Advantages
It stays cemented in the mouth and does not come out.
Disadvantages
This does involve cutting down the teeth on either side of the missing tooth to be able to connect them together. Floss threaders, which slide under the bridge, should be used daily, to keep it clean.
The disadvantages for bridges are cutting down teeth that might be perfectly healthy. If there is a leak under the anchor teeth of the bridge, decay can occur below. A bridge can replace one or two missing teeth easily, and sometimes more if there is enough support.
Removable partial denture
A removable partial denture is worn during the day. This is used to replace one or many missing teeth.
Disadvantages
-Sometimes amay need metal clasps to help it stay in the mouth which may be visible when speaking or smiling.
– They move a little when speaking or eating, which can be uncomfortable.
-We recommend taking them out at night and soaking them in a cleaning solution.
Advantages
There is no need to file down any teeth, and this option is usually the most economical. A full denture can replace all missing teeth.
Dental Implant
An implant is a great way to replace a missing tooth.
Advantages
This solution feels and acts the most like a natural tooth when chewing, brushing or smiling. A major advantage is no need to alter any other teeth when placing an implant. An implant is a great solution for a single missing tooth, and even more implants can replace many missing teeth. When smiling or talking there is no way to tell the difference between an implant and a natural tooth.
Disadvantages
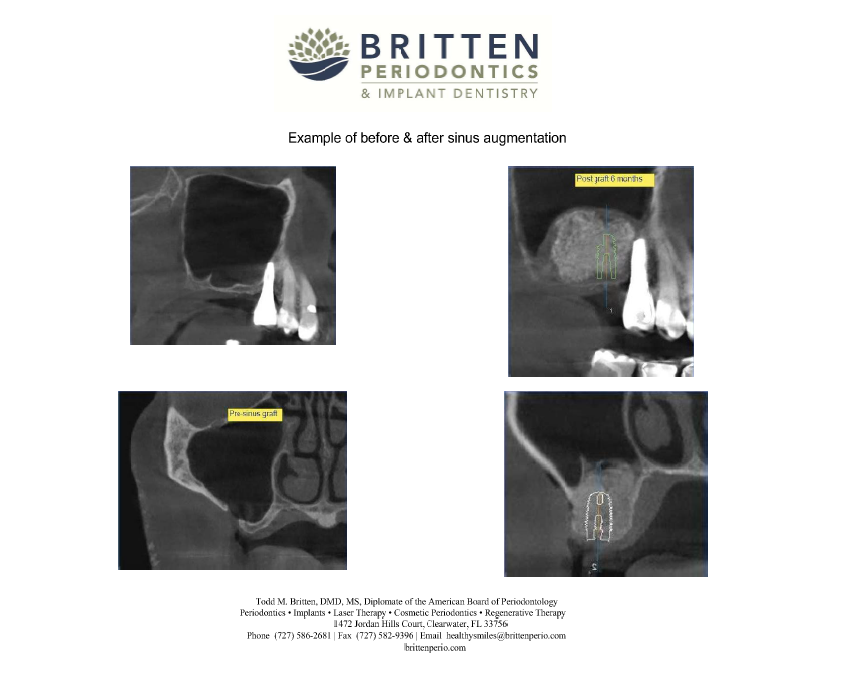
The implant replaces the actual root of the missing tooth and heals in the bone for 3 to 7 months and we then begin the restorative phase. We or your dentist then place an abutment, to which a crown will be cemented. Dental implants are usually a more costly option, at least initially, but are often the best long-term investment.
Do Nothing
There is always the option to do nothing.
Advantages
Saves money, at least initially
Disadvantages
When a tooth is removed, the bone shrinks away and the other teeth in the area will shift to fill the gap. This can sometimes lead to other problems like shifting of other teeth, causing bone loss or decay around the existing teeth as they become more difficult to clean.
If you have questions about replacing teeth lost to fractures, decay or gum disease, contact us today at 727-586-2681.
www.brittenperio.com




 [iphorm id=”3″ name=”Contact form”]
[iphorm id=”3″ name=”Contact form”]